New Study Suggests Your Cholesterol May Not Be Too High After All.
Current advice for what constitutes a healthy level of LDL ("the bad cholesterol") is incongruent with the data of 177,860 patients.
In a retrospective cohort study published in March, 2024, researchers sought to determine whether an association exists between cholesterol and long-term mortality.
Using electronic records from the University of Pittsburgh Medical Center, they looked at data from 177,860 patients aged 50 to 89 from 2000 to 2022. Patients included did not have diabetes and were not on statins. The researchers searched for connections between baseline low-density lipoproteins (LDL) and all-cause mortality.
Researchers found that patients with extremely low and extremely high levels of LDL ("the bad cholesterol") had a higher risk of long-term mortality. The lowest risk was found in patients with an LDL between 100 and 189 mg/dL, which is much higher than current recommendations, they noted.
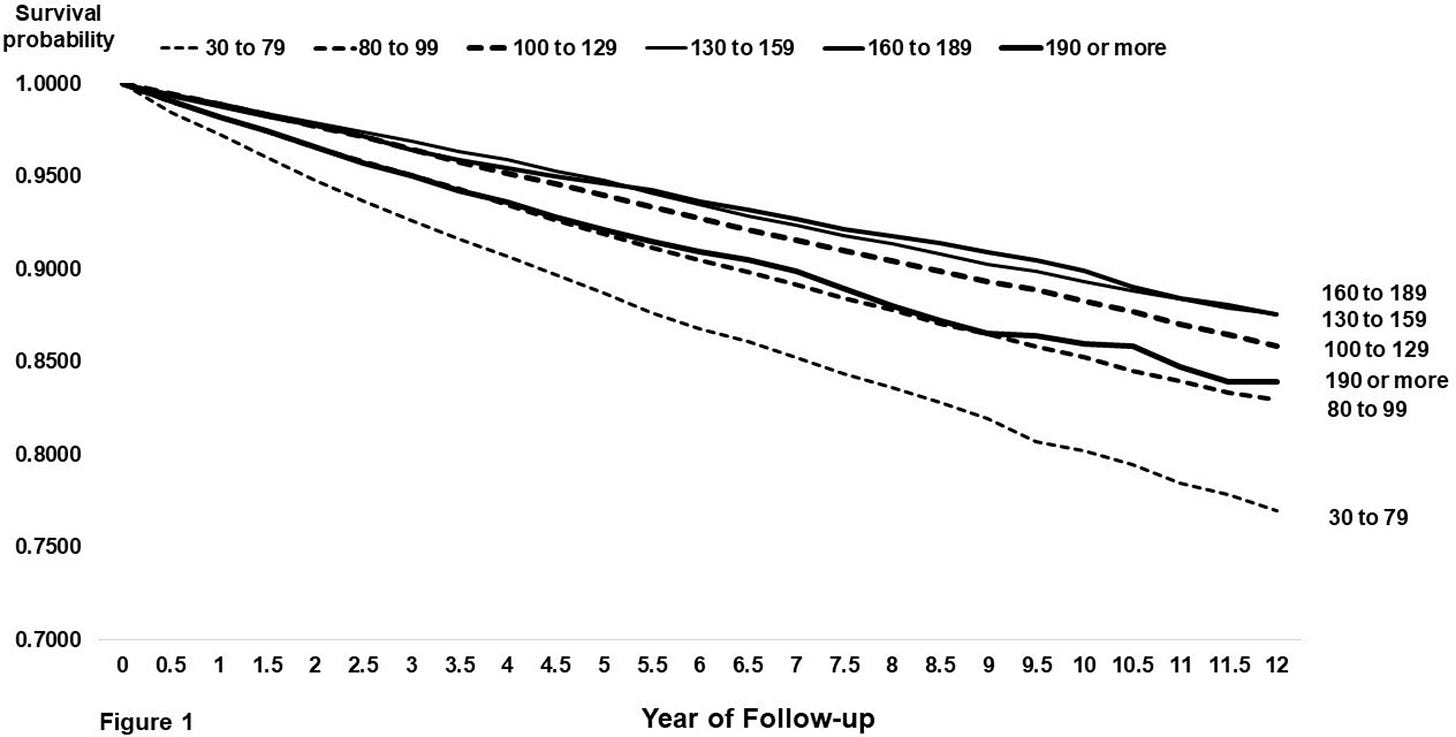
Figure 1, thanks to BMJ Open, illustrates this phenomenon. Each diagonal line on the graph is a different stratification of LDL level at baseline. As you can see, the patients with the highest probability of survival over twelve years were those with LDL between 100 and 189 mg/dL
Just as important, they found a stronger indicator of mortality to be the ratio of total cholesterol to high-density lipoproteins (HDL -- the good cholesterol). Greater than 6 was the highest risk, while less than 3 had the lowest risk.
Another more valuable indicator was the ratio of triglycerides to HDL. Patients whose ratio was 3.44 or higher had the highest risk of mortality, while those whose ratio was 1.06 or lower had the lowest risk.
The researchers concluded:
Collectively, these observations suggest that adult patients without diabetes counseled for primary prevention of ASCVD [atherosclerotic cardiovascular disease] be apprised of their estimated future risk of ASCVD with minimal consideration of their LDL-C concentration and more consideration of the T-C/HDL and triglycerides/HDL-C ratios along with other established causes of ASCVD (eg, high blood pressure, smoking, physical inactivity) and potentially coronary artery calcium scoring.
Now let's take a look at some more studies on cholesterol.
Does high cholesterol help cancer patients survive?
In January of 2024, researchers in Seoul, Korea published a longitudinal cohort study. They analyzed the data from 59,217 cancer patients between 2008 and 2019. Their findings echoed the study above.
As illustrated in the following graph thanks to Scientific Reports, an LDL of 142 mg/dL corresponded to the lowest all-cause mortality risk. Low LDL levels, on the other hand, were associated with a higher mortality risk.
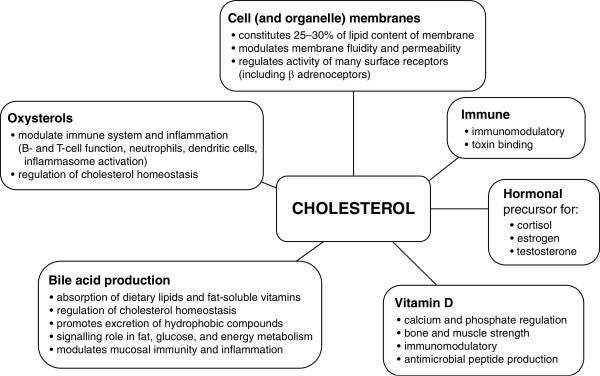
The researchers speculated that the mechanism has to do with LDL's importance to our immune systems.
In addition, they found that lower levels of HDL were significantly associated with an increased mortality risk. As such, the lowest risk of death was in patients with an HDL of greater than 61.
Then who needs to worry about high cholesterol?
Is there anyone for whom high LDL is a bad thing, as most physicians seem to assume it is for everyone? Researchers answered this question in a study published in 2023 of 23 132 patients with symptoms of coronary artery disease in Denmark. They followed them for a medium span of 4.3 years.
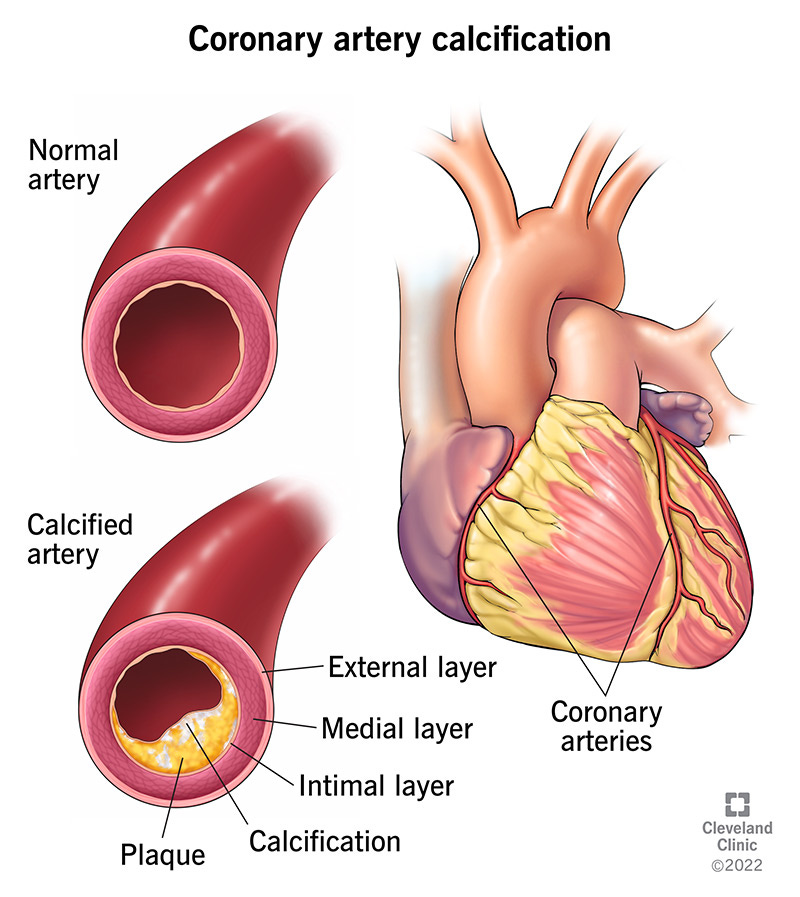
Participants were tested for coronary artery calcification using coronary computed tomography angiography. In participants with coronary artery calcification, high LDL was associated with an increased risk of myocardial infarction and ischemic stroke. In participants without coronary artery calcification, there was no association between high LDL and risk of myocardial infarction and ischemic stroke.
The following bar graph, thanks to ASA/AHA Journals, illustrates this phenomenon. The green bar represents patients without coronary artery calcium and the red represents patients with it. The vertical axis displays the number of heart attacks per excess amounts of LDL.
In other words, high LDL is only cause for concern if an individual is diagnosed with coronary artery calcification. In that case, the individual has a higher probability of having a heart attack and stroke.
Patients without coronary artery calcification are not off the hook, however. If they had low HDL levels or diabetes or were smokers, they too had an increased risk of atherosclerotic cardiovascular disease.
If you want to take a deep dive into why high LDL is only harmful if one has heart disease, this interview with Paul Saladino and Mike Fave brought several of the studies in this post to my attention. They explain that while LDL does accompany plaque, high LDL doesn't necessarily mean that someone has a lot of plaque in her arteries.
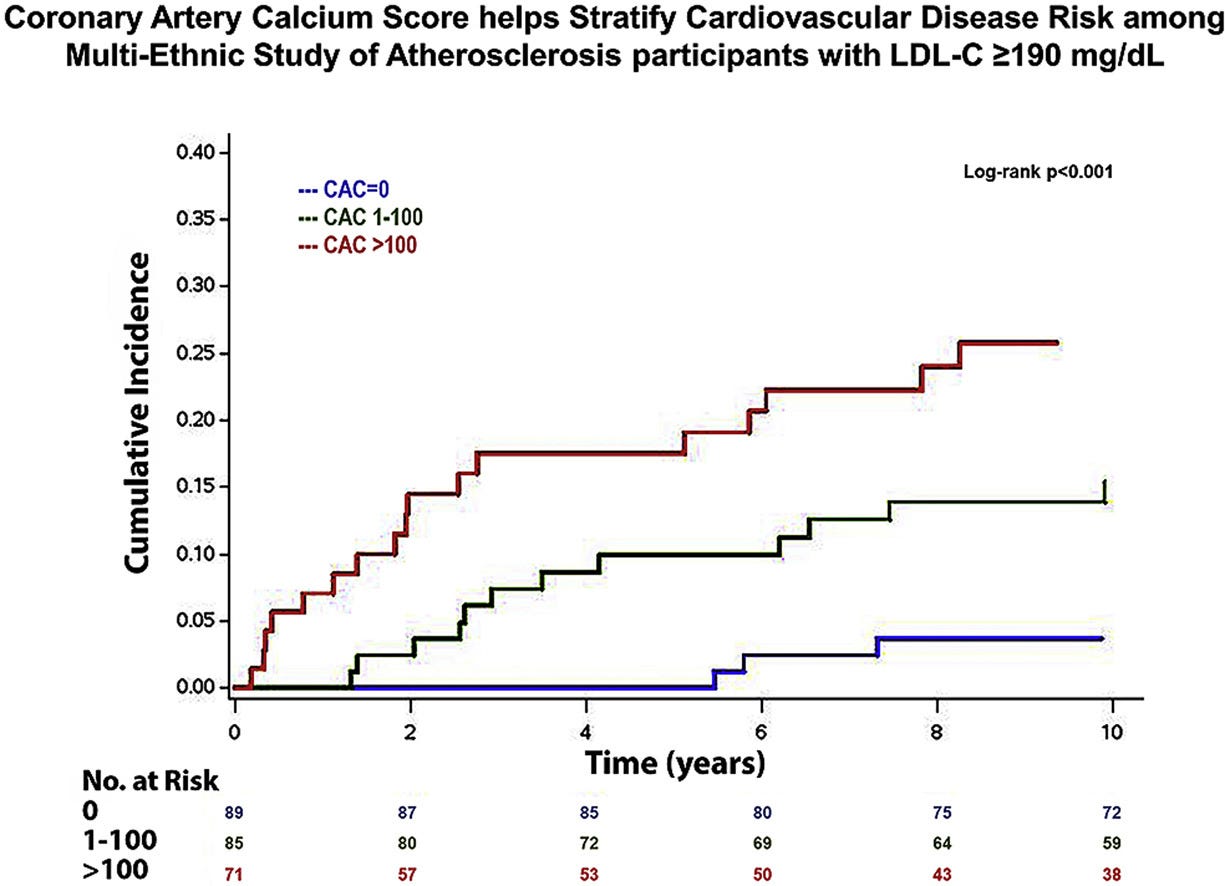
The Multi-Ethnic Study of Atherosclerosis, published in 2019, foretold the findings of the previous study. Researchers in Atlanta included 246 adults with LDL of at least 190 mg/dL (very high). The median follow-up time was 13.2 years. They discovered that those with no coronary artery calcium had a low risk of cardiovascular disease. In the following graph thanks to the journal Atherosclerosis, the vertical axis measures the cumulative incidence of cardiovascular events. The red line represents those with a high amount of coronary artery calcium, the green line represents those with a moderate amount, and the blue line represents those with none.
What factors were associated with having coronary artery calcium at baseline? Diabetes, older age, and male sex.
The study did not look at HDL.
When cholesterol-lowering meds can help
In a randomized, placebo-controlled trial conducted in Canada and the USA, 4159 patients were monitored for four to six years. All participants had experienced a heart attack before the trial. Half received the medication pravastatin, which reduced coronary death or recurrent heart attacks by 24%. Researchers found that the coronary event rate declined as LDL declined down to 125 mg/dL. However, LDL concentrations lower than 125 mg/dL were not associated with a lower risk of heart attack.
In other words, there appeared to be no benefit to lowering one's LDL level below 125 mg/dL.
What's blood sugar got to do with it?
In a 2022 review, researchers in the USA and Australia looked at studies on the relationship between cholesterol and cardiovascular disease.
The hypothesis that high levels of low-density lipoproteins (LDL) cause heart disease is inconsistently supported by evidence, they state. Furthermore, LDL is an important component of the immune system. Additionally, individuals with familial hypercholesterolemia have an equal or lower all-cause mortality rate than the rest of the population.
Cardiovascular disease develops in large part due to chronically high levels of glucose and insulin, explain the researchers. Low carbohydrate diets have demonstrated the capacity to decrease the risk of cardiovascular disease by healing metabolic syndrome, reducing adipose tissue, improving blood pressure, lowering lipoprotein(a) levels, and reducing inflammation.
Low-carb eaters' ratio of triglycerides to HDL tends to be excellent, but what about when they have high LDL? Are statins helpful under those circumstances? The answer, argue the researchers, is a resounding "no." Spotlighting two randomized, placebo-controlled clinical trials testing statins, they point out that statins had no benefit (but all of the risks) for participants with healthy ratios of triglycerides to HDL.
Echoing the studies above, they specify that HDL is a far more important datapoint in predicting cardiovascular disease than LDL. In Figure 1, the white bars represent patients with coronary heart disease, while the gray bars represent patients without it. The vertical axis is the level of lipids in their blood. As you can see, total cholesterol (TC) and LDL were similar in both patient groups. However, those without heart disease, on average, had significantly lower triglycerides (TGs) and significantly higher HDL.
People with high cholesterol live longer
In a cohort study published in 2022, researchers followed 14 035 American adults for 23 years and compared their LDL levels and mortality rates..
Participants with the lowest all-cause mortality had LDL levels between 160 and 190 mg/dL (which is currently considered too high). Participants with the second lowest all-cause mortality had LDL levels between 130 and 160 (which is currently considered slightly too high).
When only considering patients who died due to cardiovascular disease, the lowest mortality rate had an LDL of 100-130 mg/dL.
What roles does cholesterol play in the human body?
In a review published in 2022, researchers explore the role of cholesterol after a patient contracts sepsis. Cholesterol levels rise dramatically and, in survivors, gradually return to normal.
Thanks to the American Journal of Respiratory and Critical Care Medicine, the following graphic depicts the important functions of cholesterol in the human body.
COVID-19 survivors had higher cholesterol
A retrospective study published in 2021 observed the relationship between cholesterol levels and mortality rate.
When comparing 654 patients in Valladolid, Spain infected with SARS-CoV-2 in 2020, researchers found that survivors had significantly higher total cholesterol, LDL, and HDL than non-survivors.
Cholesterol levels were inversely correlated with inflammation.
People with low cholesterol still get hospitalized for coronary artery disease
In a clinical investigation published in 2009, researchers in the USA looked at records from 541 hospitals from 2000 to 2006. They found 231 986 hospitalizations for coronary artery disease and zeroed in on the 136 905 in which lipid levels were documented at admission. The mean LDL level was a relatively low 104.9 ± 39.8. Almost half of patients hospitalized for coronary artery disease had LDL levels below 100 mg/dL. The mean HDL level was 39.7 ± 13.2.
Rather than questioning the hypothesis that high cholesterol causes heart disease, the researchers shockingly concluded that the guidelines for healthy LDL levels may need to be lowered even more. In addition, they called for the development of treatments to raise HDL.
Financial conflicts of interest
Four of the researchers declared no conflicts of interest. The other four researchers, to their credit, disclosed grants or compensation from Accumetrics, AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Merck, Sanofi-Aventis, Schering Plough, Pfizer, and Abbott.
Except for the study on the pravastatin trial, which was funded by the Bristol-Myers Squibb Pharmaceutical Research Institute, the researchers in all the other papers in this post declared no competing interests.
Old news
In 1977, the Framingham Heart Study showed that having low HDL appeared to be far riskier in terms of heart disease than having high LDL.
If LDL were a tree, this is what it might look like. Why do we keep barking up the wrong tree?
Then what causes plaque to form in our blood vessels?
In her book Change Your Diet, Change Your Mind, Georgia Ede describes the importance of cholesterol.
Although the brain represents only 2% of your total body weight, it contains 20% of your body’s cholesterol . . . . Cholesterol is too big and bulky to enter the brain across the blood-brain barrier, so not a single molecule of your brain’s cholesterol comes from the cholesterol in your food. Instead, the brain makes all of its own cholesterol on-site, from scratch. I ask you: Why would the brain go out of its way to intentionally produce large quantities of a substance that’s bad for you? It wouldn't. It's really smart. It's a brain.
Cholesterol isn't what causes plaque formation, she explains. Rather, plaque builds up when the cells lining the inside of our blood vessels are damaged. Smoking, high blood glucose levels, and high blood pressure are among the culprits that can impair these cells.
Let's use Moorea's bloodwork as an example
This is a screenshot of my own blood test results. As you can see, my LDL was 158 mg/dL, which my doctor wanted to treat. However, the studies above would place that within the healthy range.
My triglycerides were 84.8 mg/dL and my HDL was 65.7 mg/dL, both of which are good (Ede).
My ratio of total cholesterol to HDL turns out to be 3.67, which is a bit higher than optimal (Kip et al.).
As far as the ratio of triglycerides to HDL, mine was 1.29. That's not so bad that I was pre-diabetic, but it leaves room for improvement. The healthiest level appears to be below 1.06 (Kip et al.).
According to Diamond et al. and Ede, minimizing my consumption of sugars and starches should get me there. Minimizing my consumption of saturated fat, on the other hand, wouldn’t make a difference.
Similarly, my fasting blood glucose was 95.1 mg/dL. According to Ede, that's not so high that I'm insulin resistant, but it would be ideal to get it down to between 70 and 85.
TL;DR
Only patients with coronary artery calcification benefit from lowering their LDL.
LDL levels lower than 100 mg/dL are associated with a higher all-cause mortality rate.
COVID-19 survivors had significantly higher cholesterol than non-survivors.
Cancer patients with low cholesterol had a significantly higher mortality rate.
An HDL of greater than 61 is associated with longevity.
A ratio of triglycerides over HDL of 1.06 or lower is associated with longevity.
If my ratio of triglycerides over HDL needs improvement, a diet with minimal sugars and starches has proven to be an effective strategy.
The current practice of prescribing statins to patients with moderate LDL levels (while telling them their cholesterol is too high) is incongruent with the science.
References
Amit Sachdeva et al., “Lipid Levels in Patients Hospitalized with Coronary Artery Disease: An Analysis of 136,905 Hospitalizations in Get With The Guidelines,” American Heart Journal 157, no. 1 (2009): 111 -7.e2, https://doi.org/10.1016/j.ahj.2008.08.010.
Aparisi Á, Iglesias-Echeverría C, Ybarra-Falcón C, et al. Low-density lipoprotein cholesterol levels are associated with poor clinical outcomes in COVID-19. Nutrition, Metabolism & Cardiovascular Diseases, 31, 9 (2021): 2619-2627. doi: 10.1016/j.numecd.2021.06.016.
Bødtker Mortensen, M., Dzaye, O., Bødtker, H.E., et al. Low-Density Lipoprotein Cholesterol Is Predominantly Associated With Atherosclerotic Cardiovascular Disease Events in Patients With Evidence of Coronary Atherosclerosis: The Western Denmark Heart Registry. Circulation 147, 14 (2023). doi.org/10.1161/CIRCULATIONAHA.122.061010.
Diamond, David M.; Bikman, Benjamin T.; Mason, Paul. Statin therapy is not warranted for a person with high LDL-cholesterol on a low-carbohydrate diet. Current Opinion in Endocrinology & Diabetes and Obesity 29, 5 (2022): 497-511, DOI: 10.1097/MED.0000000000000764
Ede, Georgia. Change Your Diet, Change Your Mind (2024). Grand Central Publishing, Kindle edition.
Gordon, T. et al., (1977). High density lipoprotein as a protective factor against coronary heart disease: The Framingham Study. The American Journal of Medicine, 62(5): 707-714.
Hofmaenner DA, Kleyman A, Press A, Bauer M, Singer M. The Many Roles of Cholesterol in Sepsis: A Review. Am J Respir Crit Care Med. 2022 Feb 15; 205(4):388-396. doi: 10.1164/rccm.202105-1197TR.
Huang, YW., Jian, ZH., Chang, HC. et al. Vegan diet and blood lipid profiles: a cross-sectional study of pre and postmenopausal women. BMC Women's Health 14, 55 (2014). doi.org/10.1186/1472-6874-14-55
Kim, S., Kim, G., Cho, S.H. et al. Association between total cholesterol levels and all-cause mortality among newly diagnosed patients with cancer. Scientific Reports 14, 58 (2024). doi.org/10.1038/s41598-023-50931-6
Kip KE, Diamond D, Mulukutla S, et al. Is LDL cholesterol associated with long-term mortality among primary prevention adults? A retrospective cohort study from a large healthcare system. BMJ Open (2024);14:e077949. doi: 10.1136/bmjopen-2023-077949
Pratik B. Sandesara et al., Clinical significance of zero coronary artery calcium in individuals with LDL cholesterol ≥190 mg/dL: The Multi-Ethnic Study of Atherosclerosis, Atherosclerosis 292 (2020): 224-229, doi.org/10.1016/j.atherosclerosis.2019.09.014
Rong, S., Li B., Chen, L. et al. Association of Low‐Density Lipoprotein Cholesterol Levels with More than 20‐Year Risk of Cardiovascular and All‐Cause Mortality in the General Population. Journal of the American Heart Association 11,15 (2022). doi.org/10.1161/JAHA.121.023690
Sacks, F.M., Moyé, L.A., Davis, B.R. et al., Relationship Between Plasma LDL Concentrations During Treatment With Pravastatin and Recurrent Coronary Events in the Cholesterol and Recurrent Events Trial, Circulation 97, 15 (1998), https://doi.org/10.1161/01.CIR.97.15.1446.








Thanks you Moorea for clearing this topic of cholesterol levels. The studies you have shown define clear boundaries for such a key substance that just for money is prescribed in patients that will have no benefits and also Rosuvastatin increase the risk of type 2 diabetes. A business that sell hundreds of billion dollars. Great work Moorea.
Loved it! This is very thorough. I was chatting with a client yesterday who asked if I was worried about my cholesterol. I said yes, "I was worried about it being low." This is such important information you've put together <3